TO OFFER YOU A BETTER EXPERIENCE, THIS SITE USES COOKIES, INCLUDING THOSE OF THIRD PARTIES. TO FIND OUT MORE, CONSULT THE PRIVACY POLICY
Prostate cancer, explained
Here’s what we need to know about the third most common cancer diagnosed among Filipino men.
By: Preferred Global Health
Prostate cancer is the second most common cancer globally diagnosed in men. In the Philippines, it is the third most frequent cancer affecting men, following lung and colorectum[i] cancers.
Although it is so widely spread, prostate cancer is not as deadly as it once was. However, the difference in treatment efficacy and impact on quality of life for men with prostate cancer varies depending on the stage of cancer in which it is detected. For this reason, it is important to increase awareness and understanding of how to prevent this cancer, detect it, and improve the health and well-being of our dads, papas, and tatays.
First things first, what’s a prostate? The prostate is a gland in males the size of a golf ball located below the bladder and in front of the rectum. It is responsible for making the fluid that forms semen. When the cancer has spread, or metastasized, beyond the prostate gland, it is considered “advanced”. It is common for cancer cells to reach the bones first.
Clarifying myths about prostate cancer
A death sentence. Survival for 10 or more years following a diagnosis of prostate cancer has improved dramatically around the world over the last 30 years. In the Philippines, there were 3, 164 deaths in 20201. This is largely due to earlier diagnosis because of increased availability of screening with improved testing for Prostate Specific Antigen (PSA) in men without symptoms of the disease as well as more effective treatments for both early and advanced cases.
Advanced cancers cannot be treated. Even if prostate cancer has advanced such that it cannot be cured by radiation or surgery, with treatment men can live a long time. New effective drugs have been introduced over the last decade and it is possible to manipulate the testosterone hormone. These treatments help make prostate cancer a more manageable chronic disease with higher survival chances and a better quality of life.
“It will not happen to me, or only when I am over 65.” While it is true that age is the principal risk factor for developing prostate cancer, there are certain prostate cancers that can be found in men as early as their forties.
The key with detection is understanding the difference between harboring a prostate cancer that will never likely cause harm and having aggressive prostate cancers that need active treatment.
Treatment may vary from what is called “active surveillance”. This includes follow-ups and regular monitoring to radiation or minimally invasive robotic assisted surgery that both have high success rates.
High PSA levels mean cancer. High levels of PSA may not be due to cancer. All prostate cells, normal or cancerous, produce PSA proteins. High levels can be made by normal prostate tissue or by prostate cancer cells. But if the PSA levels keep going up, it is likely that they are coming from cancer. Elevated levels of PSA are often referred for a biopsy or lead to further testing for cancer by urologists.
It will cause impotence or incontinence for the rest of my life. A majority of men will experience some type of erectile dysfunction for the first few months after prostate cancer treatment. Within one year after treatment, nearly all men with intact nerves will see a substantial improvement towards pre-treatment function. The reason this occurs is because of the location of the prostate next to several nerves, adjacent to the bladder, and with the urethra running through this. Men are more at risk of not fully recovering erectile or bladder function if the cancer is aggressive and widespread, meaning surgeons need a wider margin, or they undergo medical procedures not designed to minimize side effects or that are performed by physicians not proficient in the procedure. Men with other diseases that impair the ability to maintain an erection, like diabetes or vascular problems, will have a more difficult time returning to pre-treatment function. Skilled and experienced surgeons are more successful in leaving important areas intact. If dysfunction or major problems persist, urologists can help address post-surgery.
Prevention and self-care
Older age is the main risk for cancer. Meta-analyses have shown that prostate cancer risk is 2-3 times higher in men whose father or brother have had the disease, and almost 2 times higher in men with a second-degree relative, like a grandfather, uncle, nephew, or half-sibling. Studies have also shown that risk goes up about 20% in men whose mother has/had breast cancer, but this effect does not extend to men who have sisters diagnosed with breast cancer. Men exposed to pesticides have been found to have a 33% higher risk of prostate cancer compared to non-exposed groups.
While it is not possible to change factors such as genetics or age, actively managing existing health issues will help protect health and improve well-being.
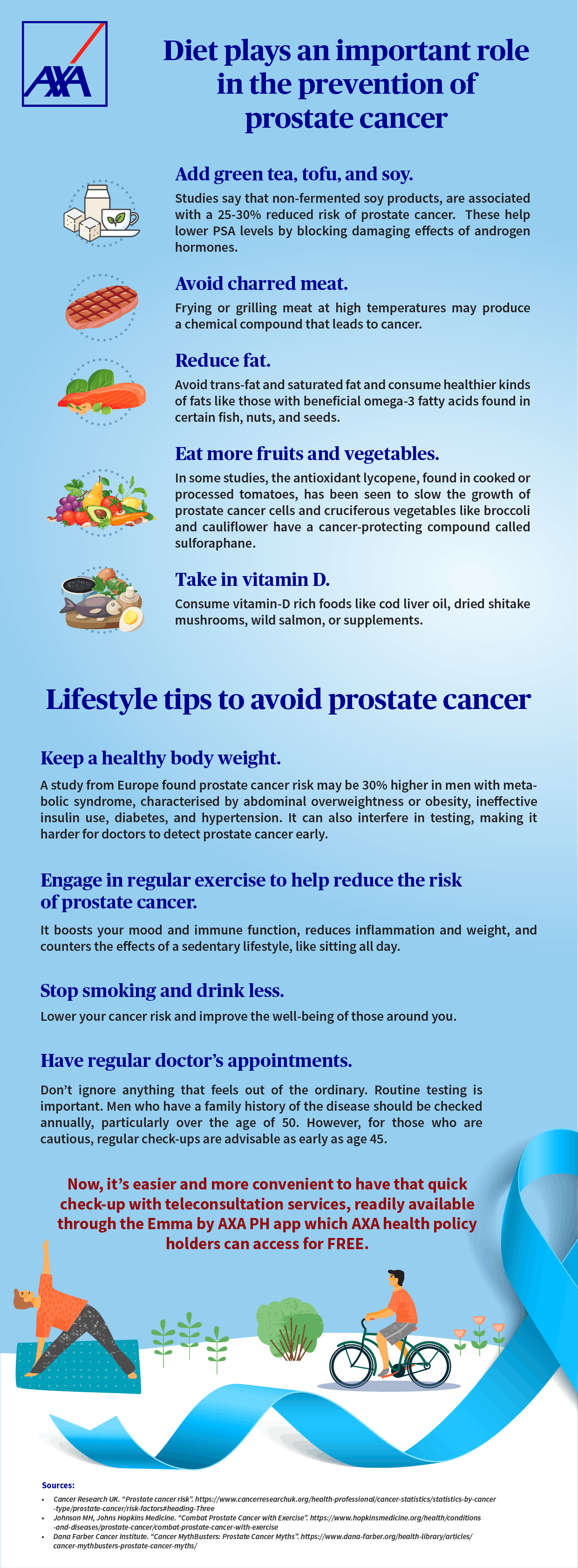
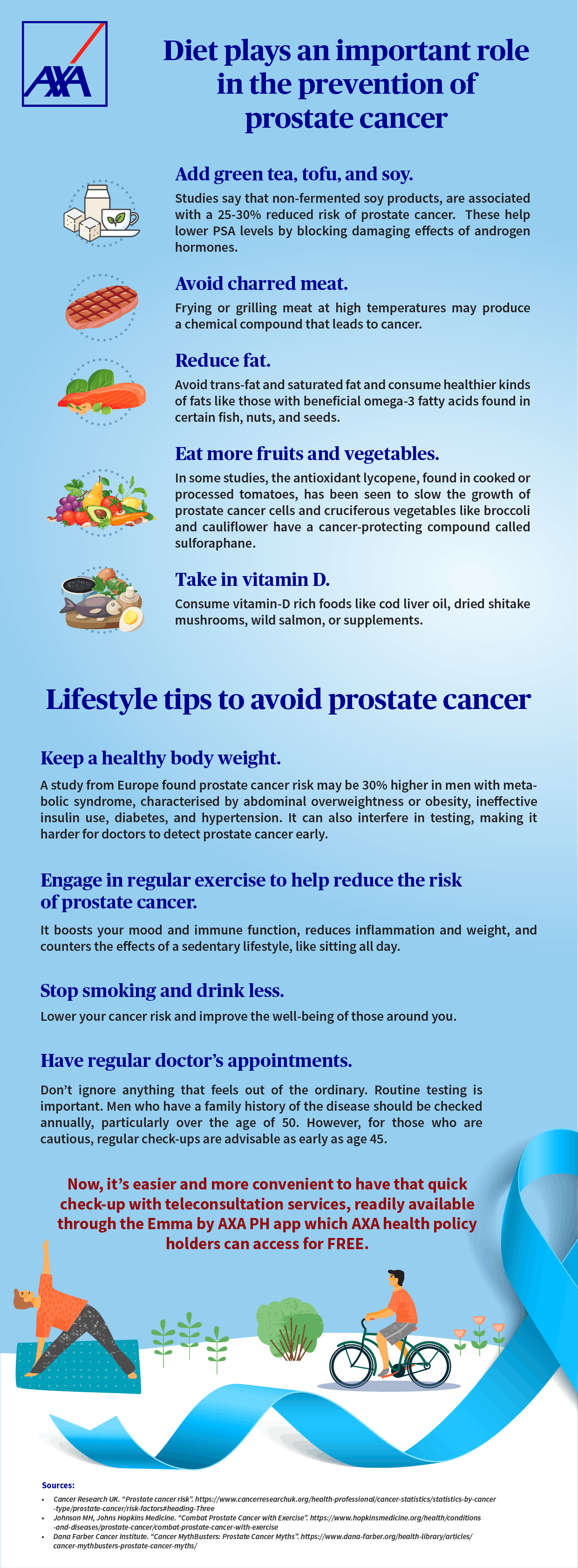
Diet plays an important role in the prevention of prostate cancer, specifically:
- Add green tea, tofu, and soy. Studies say that certain food present in Asian diets, but not as popular in the Filipino diet, like non-fermented soy products, are associated with a 25-30% reduced risk of prostate cancer[i]. Clinical trials have found that these food help lower PSA levels by blocking damaging effects of androgen hormones[ii].
- Avoid charred meat. Frying or grilling meat at high temperatures may produce a chemical compound that leads to cancer.
- Reduce fat. Avoid trans-fat and saturated fat and consume healthier kinds of fats like those with beneficial omega-3 fatty acids found in certain fish, nuts, and seeds.
- Eat more fruits and vegetables. In some studies, the antioxidant lycopene, found in cooked or processed tomatoes, has been seen to slow the growth of prostate cancer cells4. Moreover, cruciferous vegetables like broccoli and cauliflower have a cancer-protecting compound called sulforaphane.
- Take in vitamin D. Consume vitamin-D rich foods like cod liver oil, dried shitake mushrooms, wild salmon, or supplements.
Keep a healthy body weight. Obesity is linked to aggressive forms of prostate cancer and a higher chance of the cancer returning A study from Europe found prostate cancer risk may be 30% higher in men with metabolic syndrome, characterised by abdominal overweightness or obesity, ineffective insulin use, diabetes, and hypertension. It can also interfere in testing, making it harder for doctors to detect prostate cancer early.
Engage in regular exercise to help reduce the risk of prostate cancer. It boosts your mood and immune function, reduces inflammation and weight, and counters the effects of a sedentary lifestyle, like sitting all day. Furthermore, it clears your mind and helps you manage stress. Taking up a sport or performing physical activities with your kids or grandkids not only builds your overall health but your relationship with your family too.
Stop smoking and drink less. Lower your cancer risk and improve the well-being of those around you.
Have regular doctor’s appointments. Don’t ignore anything that feels out of the ordinary. Routine testing is important. Men who have a family history of the disease should be checked annually, particularly over the age of 50. However, for those who are cautious, regular check-ups are advisable as early as age 452. Methods for early detection that a urologist will recommend include a PSA test together with a digital rectal examination and an ultrasound.
Now, it’s easier and more convenient to have that quick check-up with teleconsultation services, readily available through the Emma by AXA PH app.
Cancer and other critical illnesses are not to be taken lightly since these can come unexpectedly. In such cases, AXA’s wide range of health solutions covering critical illnesses can help you prepare. Find out more by visiting AXA’s health products page by clicking here or reach out to an AXA financial partner.
Preferred Global Health (PGH) (www.pghworld.com) is a valued partner of AXA’s Preferred Consultation and Care (PCC) service. The partnership between AXA Philippines and PGH gives eligible AXA policyholders access to PCC where they can get expert advice for diagnosis verification and treatment plans from highly experienced Harvard-affiliated doctors. It provides patients the opportunity to make informed decisions in case of diagnosis of cancer and heart disease.
PGH is a leading global patient organisation based in Boston, Massachusetts, USA, with more than 20 years’ experience in patient advocacy and supporting patients and their families on the path to recovery.
Sources:
[1]Dana Farber Cancer Institute. “Cancer MythBusters: Prostate Cancer Myths”. https://www.dana-farber.org/health-library/articles/cancer-mythbusters-prostate-cancer-myths/
[1] Johns Hopkins Medicine. “Erectile dysfunction after prostate cancer”. https://www.hopkinsmedicine.org/health/conditions-and-diseases/prostate-cancer/erectile-dysfunction-after-prostate-cancer#:~:text=Nearly%20all%20men%20will%20experience,will%20see%20a%20substantial%20improvement.
[1] Cancer Research UK. “Prostate cancer risk”. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer/risk-factors#heading-Three
[1] Matias. PJM, Raymundo EM (2014) “Prostate Cancer and the Filipino: An Updated Review of Publications” J Urol Res 1(3): 1016. https://www.jscimedcentral.com/Urology/urology-1-1016.pdf
[1] Philippine Council for Health Research and Development https://www.pchrd.dost.gov.ph/index.php/r-d-updates/3208-study-reveals-increasing-incidence-of-prostate-cancer-in-developing-countries#:~:text=In%20the%20Philippines%2C%20annual%20screening,no%20symptoms%20of%20the%20disease
[1] Johns Hopkins Medicine. “Prostate Cancer: Prevention”. https://www.hopkinsmedicine.org/health/conditions-and-diseases/prostate-cancer/prostate-cancer-prevention
[1] Johnson MH, Johns Hopkins Medicine. “Combat Prostate Cancer with Exercise”. https://www.hopkinsmedicine.org/health/conditions-and-diseases/prostate-cancer/combat-prostate-cancer-with-exercise
[1] Esposito K, Chiodini P, Capuano A, et al. “Effect of metabolic syndrome and its components on prostate cancer risk: meta-analysis”. J Endocrinol Invest. 2013;36(2):132-9.
Loading Content...